Can Cervical Cancer Be Prevented? Why Concerned About Reproductive Tract Infections?
Cervical cancer remains a significant global health concern, affecting women across diverse communities and economic backgrounds. According to the World Health Organization (WHO), cervical cancer is the fourth most common cancer among women, with 604 000 new cases and 342 000 deaths reported in 2020[1]. In recent discussions surrounding cervical cancer screening, there has been a growing interest in integrating the detection of reproductive tract infections(RTIs) into screening processes. This shift in focus aims to enhance the effectiveness of cervical cancer detection and prevention.
Understanding the link between cervical cancer and reproductive tract infections is crucial. Reproductive tract infections are caused by various microbes that can affect the health of the female reproductive system. Of particular concern is the correlation between common reproductive tract microbes and Human Papillomavirus (HPV) infection. HPV is a well-established risk factor for cervical cancer, emphasizing the need to broaden the scope of screening methods.
Copyright picture from https://news.llu.edu/patient-care/cervical-cancer-basics-of-what-you-need-know
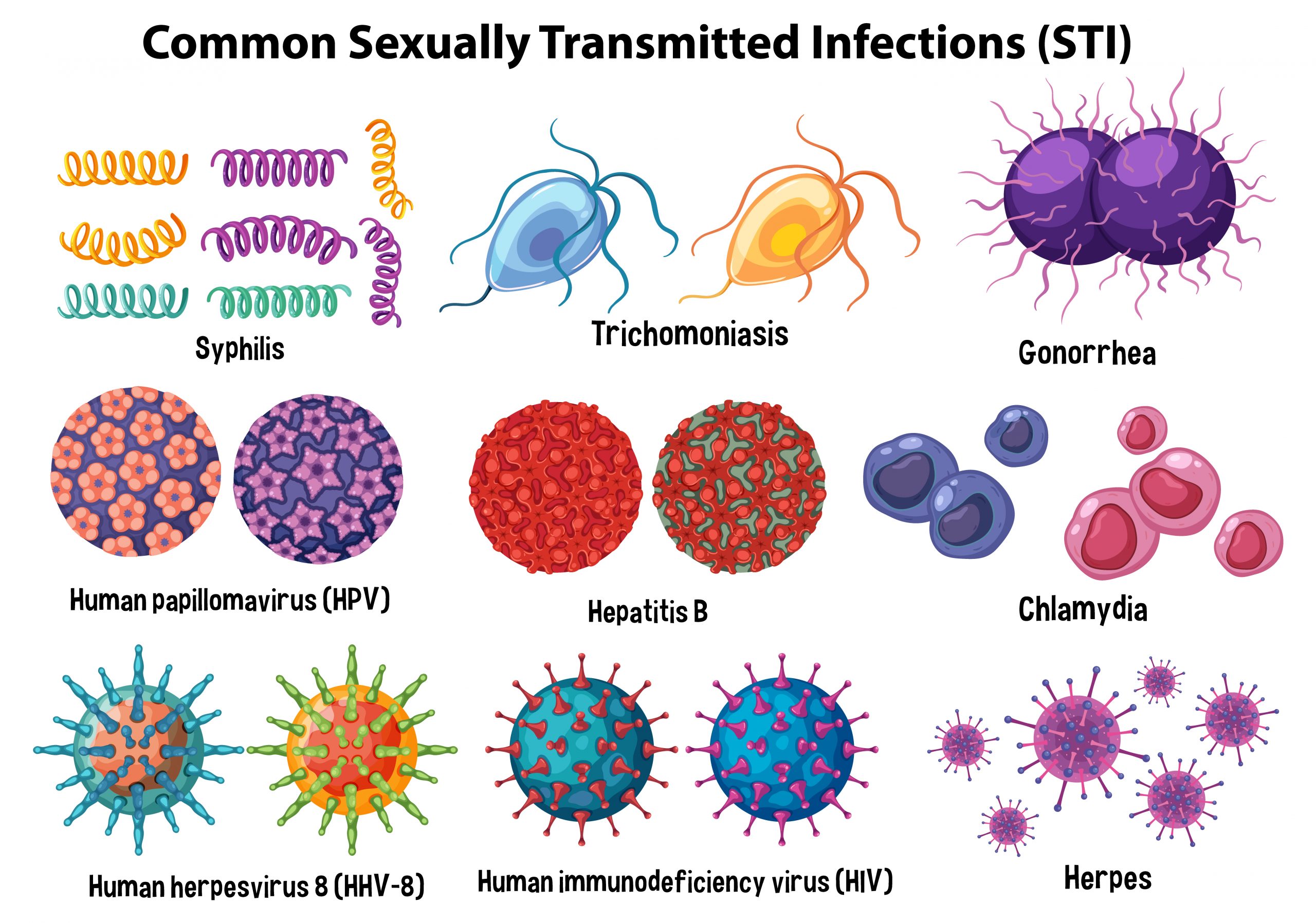
To comprehend the necessity of integrating RTI detection into cervical cancer screening, it’s essential to delve into the world of reproductive tract infections and their microbial counterparts.
Reproductive tract infections can manifest in various forms, involving microorganisms such as bacteria, viruses, and fungi. Common culprits include Chlamydia trachomatis (CT), Neisseria gonorrhoeae (NG), Mycoplasma genitalium (MG), and Ureaplasma urealyticum (UU) , etc. These microbes, when present in the reproductive tract, can lead to a range of health issues, from discomfort to more severe complications if left untreated.
Understanding the Correlation:
A crucial aspect of the discussion revolves around the intricate correlation between common reproductive tract microbes and Human Papillomavirus (HPV) infection. HPV, a prevalent sexually transmitted infection, is a recognized risk factor for the development of cervical cancer. Certain strains of HPV, especially high-risk types such as HPV-16 and HPV-18, have been linked to an increased likelihood of cervical cancer development[2].
The interaction between these microbes and HPV is multifaceted. Reproductive tract infections, by causing inflammation and compromising the integrity of the cervical epithelium, can create an environment conducive to HPV persistence and progression. Additionally, some microbes may facilitate the entry of HPV into susceptible cells, further increasing the risk of persistent infection.
Understanding this correlation is pivotal for healthcare professionals and researchers alike. It underscores the interconnected nature of reproductive health factors and emphasizes the importance of adopting a holistic approach to women’s health. As we delve deeper into the complex web of interactions between reproductive tract infections and HPV, the significance of integrated screening approaches becomes increasingly evident, heralding a new era in cervical cancer prevention and reproductive health management.
Comparative Analysis of Detection Methods for Reproductive Tract Infections
Various methods are employed for the detection of reproductive tract infections, each with its strengths and limitations. The primary methods include direct microscopy, culture, enzyme-linked immunosorbent assay (ELISA), and nucleic acid amplification tests (NAAT). While direct microscopy and culture have been traditional approaches, NAAT has emerged as a superior method due to its sensitivity and accuracy in detecting microbial DNA or RNA [3].
- Direct Microscopy: This method involves the direct examination of specimens under a microscope. However, it may lack sensitivity in detecting low microbial concentrations.
- Culture: Culturing involves growing microorganisms from a specimen in a laboratory setting. While it allows for the identification of specific microbes, it is time-consuming.
- ELISA: ELISA detects the presence of specific antigens or antibodies, but its sensitivity can vary.
- Nucleic Acid Amplification Test (NAAT): NAAT, including polymerase chain reaction (PCR), amplifies and detects the genetic material of microbes. This method is highly sensitive and specific, making it a preferred choice for accurate detection.
A Closer Look at Sansure’s RTIs testing kits
In the realm of cutting-edge diagnostic solutions, Sansure stands out with its range of testing kits designed for comprehensive RTIs detection. These kits utilize state-of-the-art nucleic acid amplification techniques, ensuring precise and reliable results. Here are some Sansure testing kits:
- Chlamydia Trachomatis/Ureaplasma Urealyticum/Neisseria Gonorrhoeae DNA Diagnostic Kit: Designed for the simultaneous detection of Chlamydia trachomatis (CT), Neisseria gonorrhoeae (NG), and Ureaplasma urealyticum (UU). The kit adopts real-time fluorescence quantitative PCR technique, aiming to support the early diagnosis of related RTI diseases.
- Chlamydia Trachomatis DNA Fluorescence Diagnostic Kit: Focused on Chlamydia trachomatis detection, providing targeted screening for this common reproductive tract infection.
- Neisseria Gonorrhoeae DNA Fluorescence Diagnostic Kit: Tailored for Neisseria gonorrhoeae detection, addressing the specific challenges associated with this microbial infection.
- Ureaplasma Urealyticum DNA Fluorescence Diagnostic Kit: Specialized in Ureaplasma urealyticum detection, contributing to a comprehensive understanding of reproductive tract health.
- Herpes Simplex Virus Type 2 DNA Fluorescence Diagnostic Kit: Targeting Herpes Simplex Virus Type 2 (HSV-2), this kit aids in identifying HSV-2-DNA in samples, supporting early diagnosis of venereal diseases.
Conclusion
The observed correlation between common genital microbiota and human papillomavirus (HPV) infection already underscores the necessity of combining reproductive tract infections detection with cervical cancer screening.
And we, Sansure, will keep contributing to the ongoing efforts to enhance women’s health and reduce the global burden of cervical cancer.
Reference