Diagnostic and Management Challenges of Respiratory Infections in Children
Acute respiratory infection (ARI) is the leading cause of morbidity and mortality worldwide in children under five. According to the World Health Organization statistics, about 2 million children under the age of 5 die due to ARI yearly, accounting for 20% of the total number of deaths of children under the age of 5 in the world.
An acute respiratory infection has obvious seasonality, often resulting in a sudden increase in hospital outpatient visits in a short time. Therefore, accurate identification of respiratory tract infections and formulation of appropriate diagnosis and treatment strategies are important issues facing medical workers today. The following article focuses on the presentation of respiratory tract infections in children, the current challenges in diagnosing respiratory infections, and discusses 3 different diagnostic methods.

Children’s respiratory tract infections overview
Viruses cause approximately 80% of respiratory infections in children. The main causes of viral respiratory infections include influenza, respiratory syncytial (RSV), rhinovirus, coronavirus, and more.
In most cases, respiratory infections in children are transmitted through the respiratory tract, digestive tract, or close contact. For instance, when a child’s hands come into contact with an infected person’s eye or nasal secretions that contain the virus, the virus can enter the child’s respiratory tract and create a new infection.
– Influenza
Influenza (flu) is a viral infection of the lungs and airways caused by influenza viruses. Flu is classified into three types, A, B, and C, and different types cause regular seasonal flu outbreaks. Type A and B viruses cause 70% of typical seasonal flu, and type C occurs less frequently, mainly in children.
Flu symptoms usually cause fever, sore throat, cough, headache, and muscle aches. Additionally, the most common complication of influenza is pneumonia. The virus can spread from the respiratory tract to the lungs and form viral pneumonia. Additionally, patients will experience aggravated cough, difficulty breathing, and recurrent fever. Children under 2 years of age are at particularly high risk of contracting flu complications and dying.
– Respiratory syncytial virus
Respiratory syncytial virus (RSV) is one of young children’s most common causes of acute lower respiratory tract infection. According to the CDC report on RSV in 2022, an estimated 58,000-80,000 children under the age of 5 are hospitalized each year in the United States due to RSV infection. About 60%-70% of children are infected with RSV at 1 year old, making RSV the leading cause of mortality and morbidity in children under 5 years old.
Initial RSV infection usually progresses from upper to lower respiratory tract disease with congestion and fever. The most common symptom is bronchiolitis, which can cause pneumonia with cough and difficulty breathing. Furthermore, children with bronchiolitis are more likely to be diagnosed with asthma when they grow up.
– Covid-19
Coronavirus disease (COVID-19) is an infectious disease caused by SARS-CoV-2. The virus is mainly spread from person to person through droplets produced when an infected person coughs, sneezes or talks. Common symptoms of COVID-19 include fever, cough, loss of taste and smell, muscle aches, and more.
According to UNICEF, more than 5 million children, including 2.4 million newborns and 2.2 million children and youth aged 5 to 24, have died since the start of the pandemic. In addition, certain conditions may increase children’s risk of severe illness from COVID-19, including obesity, diabetes, asthma, and congenital heart disease.
Challenges in the diagnosis of the respiratory viral pathogens
Although diagnostic techniques for viral pathogens are accepted and applied in more and more hospitals, the nonspecific clinical manifestations of respiratory infections pose considerable challenges to the differential diagnosis of these pathogens.
Most respiratory viruses lacked specific therapeutic drugs, and clinicians judged viral infections based on blood routine. Because some clinicians think the accurate diagnosis of viral pathogens is of little significance, this kind of thinking hinders the accurate diagnosis of viral etiology.
Furthermore, the specimen collection staff should carry out systematic training, and the inspectors should conduct a preliminary assessment of the sent specimens to see whether they have collected specimens that meet the requirements.
Diagnostic methods
Early and accurate diagnosis of the causative pathogen of respiratory tract infection is critical for implementing appropriate antiviral or antibacterial therapy, initiating effective infection control measures, and shortening the length of hospital stay.
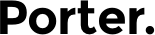
– Antigen detection assays
Antigen tests are immunoassays that detect the presence of specific viral antigens. Rapid immunoassays (RIA) take a sample from the nose or throat, and can provide test results in less than 30 minutes. RIAs are inexpensive and easy to perform. Currently, RIAs are mostly limited to detecting influenza A, B virus, and RSV.
– Serological test
Serological testing, usually taken from a finger or arm, and can identify most respiratory pathogens, such as RSV, adenovirus, influenza A, and B. Serological test can also detect coinfections in hospitalized children with acute respiratory infections other than infants. Nevertheless, serological testing has limited clinical utility compared with PCR and cannot identify frequently recurring viral infections.
– NAAT
A nucleic acid amplification test (NAAT) is a method of swabbing the nose or saliva and testing for current infection with the SARS-CoV-2 virus. It can detect COVID-19 variants, including delta variants and omicron variants. Since the beginning of the COVID-19 pandemic, NAAT, authorized by the U.S. Food and Drug Administration (FDA), has been considered the “gold standard” for determining whether adults and children are infected with COVID-19. The PCR test is considered the most accurate NAAT test, and PCR tests are less likely to produce errors than antigen tests.
Sansure: SARS-CoV-2, Influenza Virus and Respiratory Syncytial Virus Multiple Nucleic Acid Diagnostic Kit (PCR-Fluorescence Probing)

Respiratory tract infection has always been an important issue of concern worldwide. Sansure Biotech Inc. is committed to becoming a gene technology provider, offering solutions for respiratory pathogen detection. Sansure’s respiratory pathogen detection solutions allow rapid and accurate identification of pathogens and diagnostic evidence for co-infected pathogens. SARS-CoV-2, Influenza Virus and Respiratory Syncytial Virus Multiple Nucleic Acid Diagnostic Kit (PCR-Fluorescence Probing) is a real-time RT-PCR test newly developed by Sansure. This nasopharyngeal and oropharyngeal swab uses one-tube fast-release and advanced magnetic beads technology. The test results for 3 respiratory pathogens (SARS-CoV-2, Flu, RSV) can be obtained with 1 RT-PCR test. In addition, the kit’s sensitivity can be as high as 500 copies/m, which can help clinical laboratory personnel accurately detect 3 respiratory pathogens.
Contact us for more information about Sansure respiratory tract infections solutions.
Reference:
[1] Children aged <5 years with acute respiratory infection (ARI) symptoms taken to facility (%).
Available at: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/3147
[2] RSV in Infants and Young Children
Available at: https://www.cdc.gov/rsv/high-risk/infants-young-children.html
[3] COVID-19 and children
Available at: https://data.unicef.org/covid-19-and-children/
[4] Nucleic Acid Amplification Tests (NAATs)
Available at: https://www.cdc.gov/coronavirus/2019-ncov/lab/naats.html